Monkeypox is a viral zoonosis (a virus transmitted to humans from animals) with symptoms similar to those seen in the past in smallpox patients, although it is clinically less severe. With the eradication of smallpox in 1980 and the subsequent cessation of smallpox vaccination, monkeypox has emerged as the most important orthopoxvirus for public health
In 2022, the outbreak of human monkeypox (HMPX) occurred in many non-endemic countries. World Health Organization (WHO) assesses that this outbreak is “atypical”. The history of monkeypox and HMPX must be reviewed to clearly recognize the “typical” outbreaks to fully understand this comment. Therefore, this paper reviews the epidemiological history of monkeypox, especially HMPX, and discusses and analyzes the atypical manifestations and the possible causes of the present outbreak based on the recent views of WHO, other organizations/institutions, and experts. The text describes the thought-provoking history of the interaction between the monkeypox virus and the human being in the past 64 years and provides various information and views on the outbreak of HMPX, which is helpful to understand risk assessment and the potential impact of this outbreak on clinical and public health in future.
History of Monkeypox
Historically, MPXV has long been endemic in regions of sub-Saharan Africa; hence, researchers knew little about its ecology, epidemiology, and transmission. However, the World Health Organization (WHO) declared the 2022 MPXV outbreak a public health emergency of international concern soon after ~52,090 confirmed MPXV cases across 100 countries. Perhaps the current MPXV outbreak has been sustained due to efficient human-to-human transmission.
An infectious poxvirus that causes fever, chills and rashes, the disease is endemic, or consistently regionally present, in ten African countries. Until recently, however, it was rarely found in Europe and the Americas—a trend that has, historically, led Western public health officials to disregard its spread elsewhere.
The pathogen
Monkeypox virus is an enveloped double-stranded DNA virus that belongs to the Orthopoxvirus genus of the Poxviridae family. There are two distinct genetic clades of the monkeypox virus: the central African (Congo Basin) clade and the west African clade. The Congo Basin clade has historically caused more severe disease and was thought to be more transmissible. The geographical division between the two clades has so far been in Cameroon, the only country where both virus clades have been found.
The natural host of monkeypox virus
Various animal species have been identified as susceptible to monkeypox virus. This includes rope squirrels, tree squirrels, Gambian pouched rats, dormice, non-human primates and other species. Uncertainty remains on the natural history of monkeypox virus and further studies are needed to identify the exact reservoir(s) and how virus circulation is maintained in nature.
Outbreaks
Human monkeypox was first identified in humans in 1970 in the Democratic Republic of the Congo in a 9-month-old boy in a region where smallpox had been eliminated in 1968. Since then, most cases have been reported from rural, rainforest regions of the Congo Basin, particularly in the Democratic Republic of the Congo and human cases have increasingly been reported from across central and west Africa.
Since 1970, human cases of monkeypox have been reported in 11 African countries: Benin, Cameroon, the Central African Republic, the Democratic Republic of the Congo, Gabon, Cote d’Ivoire, Liberia, Nigeria, the Republic of the Congo, Sierra Leone and South Sudan. The true burden of monkeypox is not known. For example, in 1996–97, an outbreak was reported in the Democratic Republic of the Congo with a lower case fatality ratio and a higher attack rate than usual. A concurrent outbreak of chickenpox (caused by the varicella virus, which is not an orthopoxvirus) and monkeypox was found, which could explain real or apparent changes in transmission dynamics in this case. Since 2017, Nigeria has experienced a large outbreak, with over 500 suspected cases and over 200 confirmed cases and a case fatality ratio of approximately 3%. Cases continue to be reported until today.
MPXV ecological habitats
Ecological niche models (ENMs) have found rope squirrels (Funisciurus spp.), but not giant pouched rats, a significant predictor of MPXV’s geographical range. Accordingly, ENM-predicted areas have more MPXV cases in humans, as confirmed by epidemiological studies. MPXV is the only known orthopox virus (OPXV) circulating in West and Central Africa, yet, the possible presence of other OPXVs hinders measurements of MPXV prevalence. Researchers have isolated MPXV from a rope squirrel and a chimpanzee, but no study has documented reverse spillover in domestic animals. The recent detection of OPXV antibodies in a domestic pig in the Democratic Republic of Congo (DRC) pointed to the zoonotic and cross-species potential of OPXVs. Overall, the range of the reservoir host complex of MPXV remains unknown.
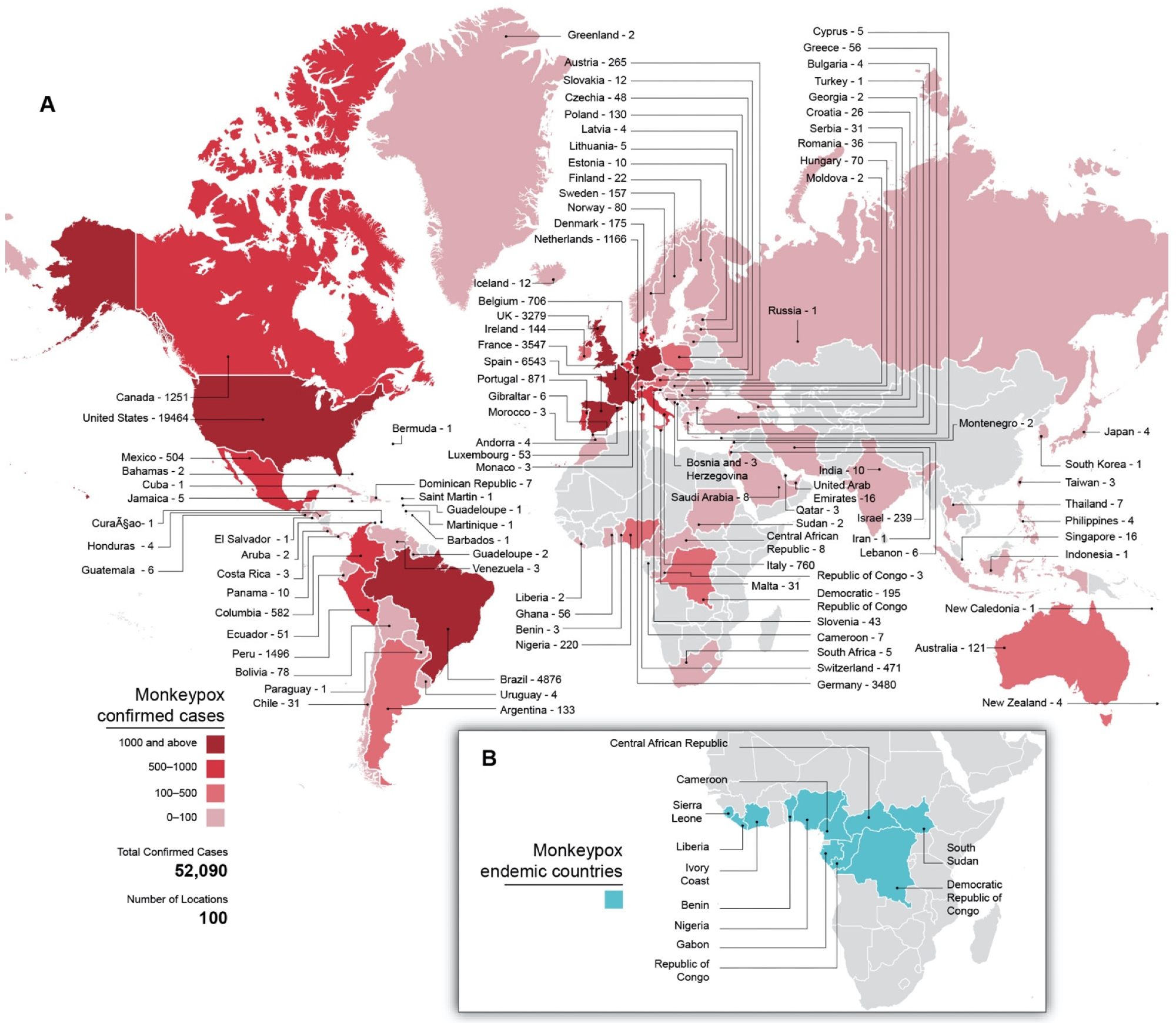 Global distribution of MPX cases. (A) MPX cases per country in the current outbreak through 1 September 2022, as well as total, confirmed cases and affected countries. Countries are coloured according to case counts. Grey shading indicates no known cases. (B) Countries historically endemic for MPXV. Grey shading indicates non-endemic countries.
Global distribution of MPX cases. (A) MPX cases per country in the current outbreak through 1 September 2022, as well as total, confirmed cases and affected countries. Countries are coloured according to case counts. Grey shading indicates no known cases. (B) Countries historically endemic for MPXV. Grey shading indicates non-endemic countries.
Transmission
Animal-to-human (zoonotic) transmission can occur from direct contact with the blood, bodily fluids, or cutaneous or mucosal lesions of infected animals. In Africa, evidence of monkeypox virus infection has been found in many animals including rope squirrels, tree squirrels, Gambian pouched rats, dormice, different species of monkeys and others. The natural reservoir of monkeypox has not yet been identified, though rodents are the most likely. Eating inadequately cooked meat and other animal products of infected animals is a possible risk factor. People living in or near forested areas may have indirect or low-level exposure to infected animals.
The ongoing 2022 MPXV outbreak unfolded atypically, showing exponential growth with low case fatality ratio (CFRs) and continuous human-to-human transmission. The estimated reproduction number of MPXV was 2.43 in Italy but rose to 1.29 through July 2022. Sequencing data have confirmed that clade 2B MPXV undergoing continuous microevolution caused the recent outbreak. Notably, MPXV has spread outside the endemic areas, disproportionately affecting men-having-sex-with-men (MSM).
Signs and symptoms
The incubation period (interval from infection to onset of symptoms) of monkeypox is usually from 6 to 13 days but can range from 5 to 21 days.


The infection can be divided into two periods:
- the invasion period (lasts between 0–5 days) is characterized by fever, intense headache, lymphadenopathy (swelling of the lymph nodes), back pain, myalgia (muscle aches) and intense asthenia (lack of energy). Lymphadenopathy is a distinctive feature of monkeypox compared to other diseases that may initially appear similar (chickenpox, measles, smallpox)
- the skin eruption usually begins within 1–3 days of the appearance of fever. The rash tends to be more concentrated on the face and extremities rather than on the trunk. It affects the face (in 95% of cases), and palms of the hands and soles of the feet (in 75% of cases). Also affected are oral mucous membranes (in 70% of cases), genitalia (30%), and conjunctivae (20%), as well as the cornea. The rash evolves sequentially from macules (lesions with a flat base) to papules (slightly raised firm lesions), vesicles (lesions filled with clear fluid), pustules (lesions filled with yellowish fluid), and crusts which dry up and fall off. The number of lesions varies from a few to several thousand. In severe cases, lesions can coalesce until large sections of skin slough off.
Vaccines
Two vaccines may be used for the prevention of monkeypox disease:
- JYNNEOS vaccine is used for the prevention of smallpox and monkeypox disease among people determined to be at high risk for infection.
- ACAM2000 vaccine is approved for immunization against smallpox disease for people determined to be at high risk for infection. It has been made available for use against monkeypox in the current outbreak.
JYNNEOS is a third-generation vaccine based on a live, attenuated non-replicating orthopoxvirus, Modified Vaccinia Ankara (MVA). MVA is a live virus that does not replicate efficiently in humans. JYNNEOS is known internationally as Imvamune or Imvanex, and is manufactured by Bavarian Nordic.
The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) for the emergency use of JYNNEOS for:
- Active immunization by intradermal injection for prevention of monkeypox disease in individuals 18 years of age and older determined to be at high risk for monkeypox infection.
- Active immunization by subcutaneous injection for prevention of monkeypox disease in individuals less than 18 years of age determined to be at high risk for monkeypox infection.
ACAM2000 is a second-generation vaccine indicated for the prevention of smallpox disease. It has been made available for use against monkeypox in the current outbreak under an Expanded Access Investigational New Drug (EA-IND) protocol, which requires informed consent along with completing additional forms. ACAM2000 contains a live vaccinia virus that is replication-competent in humans. ACAM2000 is manufactured by Emergent BioSolutions.
Available evidence supporting the use of smallpox vaccine for monkeypox prevention is derived from the vaccine used during smallpox eradication, Dryvax. Dryvax was a first-generation smallpox vaccine manufactured by Wyeth laboratories that is no longer available. Routine use of this vaccine was stopped in 1972 after smallpox was eradicated from the United States. The license was withdrawn in 2008 and no supplies of this vaccine remain.
Globally and in the United States, the supply of JYNNEOS vaccine is currently limited, although more are expected in the coming weeks and months. The United States has a large supply of ACAM2000, but this vaccine has more side effects and contraindications than JYNNEOS.
Journal reference: Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious, https://doi.org/10.3390/v14092012, https://www.mdpi.com/1999-4915/14/9/2012/htm